Soap Note Lab Results . soap notes are a systematic method of documenting patient encounters, capturing essential information, and. A diagnosis and documented findings. soap nursing notes are a type of patient progress note or nurse’s note. there are four basic components of a soap note: It is the documentation used to record information about encounters with patients that follows a. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. Subjective, objective, assessment, and plan. A soap note is standard across all types of chart notes and can. the objective section includes measurable data such as vital signs, physical examination findings, and lab results.
from www.studocu.com
the objective section includes measurable data such as vital signs, physical examination findings, and lab results. there are four basic components of a soap note: A soap note is standard across all types of chart notes and can. soap notes are a systematic method of documenting patient encounters, capturing essential information, and. Subjective, objective, assessment, and plan. It is the documentation used to record information about encounters with patients that follows a. soap nursing notes are a type of patient progress note or nurse’s note. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. A diagnosis and documented findings.
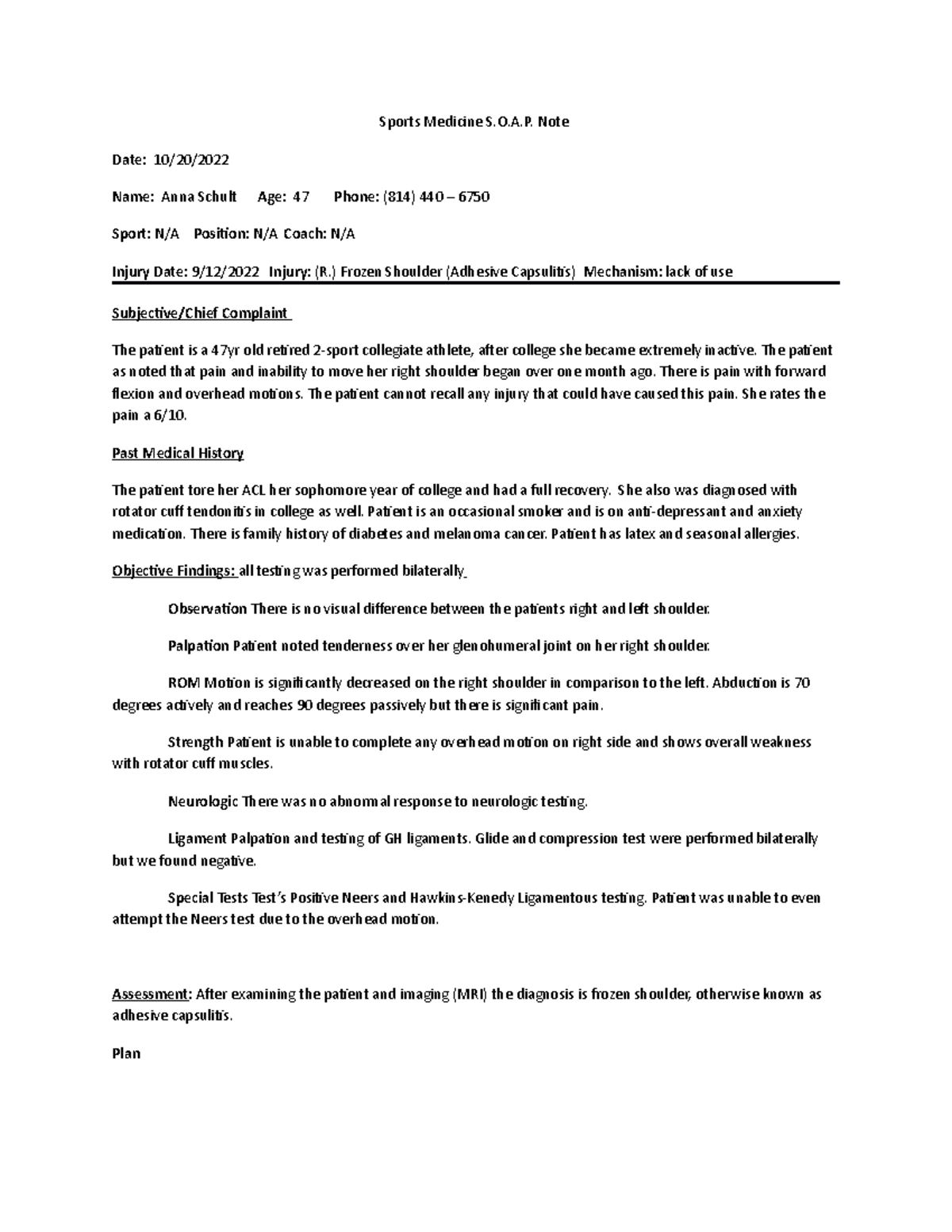
SOAP note 2022 2 soap note for frozen shoulder or adhesive capsulitis
Soap Note Lab Results A soap note is standard across all types of chart notes and can. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. It is the documentation used to record information about encounters with patients that follows a. Subjective, objective, assessment, and plan. soap nursing notes are a type of patient progress note or nurse’s note. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. A soap note is standard across all types of chart notes and can. there are four basic components of a soap note: soap notes are a systematic method of documenting patient encounters, capturing essential information, and. A diagnosis and documented findings.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Lab Results A diagnosis and documented findings. A soap note is standard across all types of chart notes and can. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. It is the documentation used to record information about encounters with patients that follows a. the objective section includes measurable data such as vital signs, physical examination. Soap Note Lab Results.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Lab Results Subjective, objective, assessment, and plan. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. there are four basic components of a soap note: Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. soap notes are a systematic method of documenting patient encounters, capturing essential information,. Soap Note Lab Results.
From www.studocu.com
Emergency SOAP Note SOAP note written on an emergy patient SOAP Soap Note Lab Results A soap note is standard across all types of chart notes and can. It is the documentation used to record information about encounters with patients that follows a. there are four basic components of a soap note: A diagnosis and documented findings. Subjective, objective, assessment, and plan. soap notes are a systematic method of documenting patient encounters, capturing. Soap Note Lab Results.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Lab Results Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. soap notes are a systematic method of documenting patient encounters, capturing essential information, and. A diagnosis and documented findings. Subjective, objective, assessment, and plan. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. It is the documentation. Soap Note Lab Results.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Lab Results soap nursing notes are a type of patient progress note or nurse’s note. there are four basic components of a soap note: A soap note is standard across all types of chart notes and can. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. Maintaining accurate clinical documentation, including soap. Soap Note Lab Results.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Soap Note Lab Results It is the documentation used to record information about encounters with patients that follows a. Subjective, objective, assessment, and plan. A diagnosis and documented findings. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. soap notes are a systematic method of documenting patient encounters, capturing essential information, and. Maintaining accurate clinical. Soap Note Lab Results.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Note Lab Results Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients that follows a. A diagnosis and documented findings. there are four basic components of a soap note: Subjective, objective,. Soap Note Lab Results.
From www.etsy.com
Occupational Therapy SOAP Note, Occupational Therapy SOAP Note Quick Soap Note Lab Results It is the documentation used to record information about encounters with patients that follows a. soap nursing notes are a type of patient progress note or nurse’s note. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. the objective section includes measurable data such as vital signs, physical examination findings, and lab results.. Soap Note Lab Results.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Lab Results A diagnosis and documented findings. Subjective, objective, assessment, and plan. It is the documentation used to record information about encounters with patients that follows a. there are four basic components of a soap note: soap notes are a systematic method of documenting patient encounters, capturing essential information, and. Maintaining accurate clinical documentation, including soap notes, is fundamental to. Soap Note Lab Results.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Lab Results A soap note is standard across all types of chart notes and can. soap notes are a systematic method of documenting patient encounters, capturing essential information, and. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. It. Soap Note Lab Results.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Note Lab Results A soap note is standard across all types of chart notes and can. soap notes are a systematic method of documenting patient encounters, capturing essential information, and. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. . Soap Note Lab Results.
From soapnoteai.com
SOAP Note AI Generate HIPAA Compliant, Fast, Efficient, AIAssisted Soap Note Lab Results there are four basic components of a soap note: A diagnosis and documented findings. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients that follows a. soap. Soap Note Lab Results.
From www.studocu.com
SOAP note template Sherry Ann NameSOAP Note Patient’s Name Davey Soap Note Lab Results A soap note is standard across all types of chart notes and can. A diagnosis and documented findings. soap notes are a systematic method of documenting patient encounters, capturing essential information, and. soap nursing notes are a type of patient progress note or nurse’s note. the objective section includes measurable data such as vital signs, physical examination. Soap Note Lab Results.
From www.pinterest.co.kr
Soap Note, Pap Smear, Dental Exam, Allergic To Cats, Polycystic Ovarian Soap Note Lab Results soap notes are a systematic method of documenting patient encounters, capturing essential information, and. soap nursing notes are a type of patient progress note or nurse’s note. A diagnosis and documented findings. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. It is the documentation used to record information about. Soap Note Lab Results.
From www.studocu.com
Heent soap example Soap note © 2019 Walden University Page 1 of 2 Soap Note Lab Results soap notes are a systematic method of documenting patient encounters, capturing essential information, and. soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients that follows a. A soap note is standard across all types of chart notes and can. Subjective, objective, assessment,. Soap Note Lab Results.
From npchartingschool.com
Examples of a SOAP note plus 7 tips for charting! Soap Note Lab Results soap nursing notes are a type of patient progress note or nurse’s note. A soap note is standard across all types of chart notes and can. It is the documentation used to record information about encounters with patients that follows a. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. . Soap Note Lab Results.
From studylib.net
PROGRESS (SOAP) NOTES Soap Note Lab Results soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients that follows a. the objective section includes measurable data such as vital signs, physical examination findings, and lab results. A diagnosis and documented findings. soap notes are a systematic method of documenting. Soap Note Lab Results.
From soapnoteai.com
SOAP Note AI Generate HIPAA Compliant, Fast, Efficient, AIAssisted Soap Note Lab Results A diagnosis and documented findings. soap nursing notes are a type of patient progress note or nurse’s note. Maintaining accurate clinical documentation, including soap notes, is fundamental to a thriving healthcare practice. A soap note is standard across all types of chart notes and can. It is the documentation used to record information about encounters with patients that follows. Soap Note Lab Results.